Thousands of patients and health care workers were infected during COVID-19 outbreaks in acute care facilities in Alberta in the last year, raising questions about why more isn’t being done to prevent in-hospital transmission.
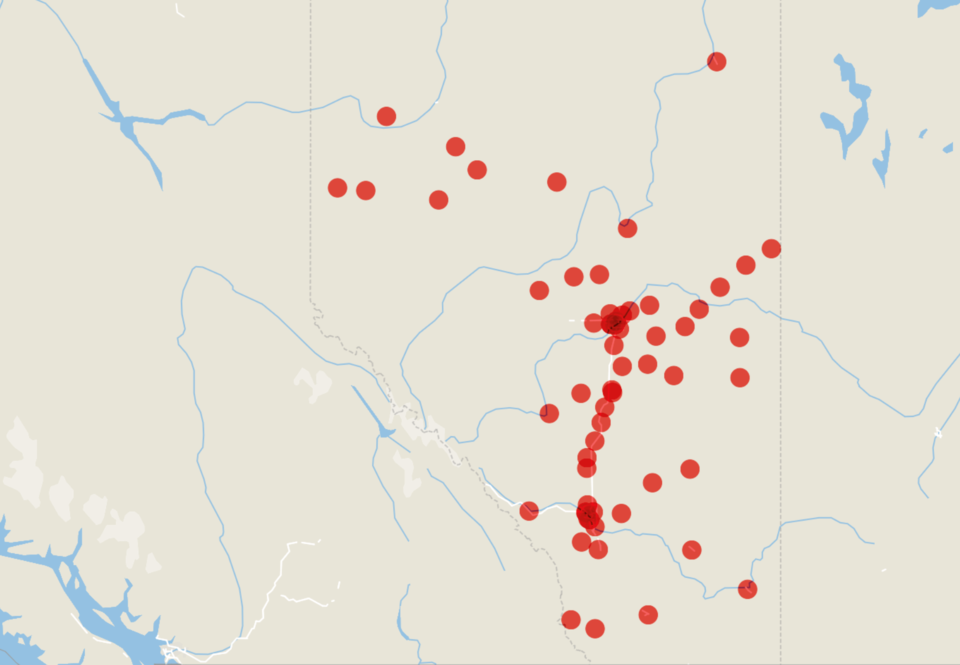
Between Sept. 1, 2023, and Aug. 31, 2024, more than 300 COVID-19 outbreaks were declared at Alberta Health Services and Covenant Health acute care facilities throughout the province, according to data from AHS obtained through a freedom of information request.
In the largest outbreak, a single University of Alberta Hospital unit reported 43 infected patients in November 2023. Though outbreaks were more common in Alberta’s largest hospitals, no part of the province was unaffected. In total, 63 separate acute care facilities reported outbreaks, including incidents involving more than 20 people in Athabasca, Lamont, and Wetaskiwin.
During these outbreaks, 2,352 patients and 660 health care workers tested positive for COVID.
Dr. Joe Vipond, an emergency physician in Calgary and co-founder of the Canadian Covid Society, said it is worrisome that patients are being harmed and that steps aren't taken to adequately protect them.
“The reality is that people are dying from COVID in our hospitals, and we really are doing very little to prevent them getting ill and getting infected. And we wouldn't do the same for any other infectious disease,” Vipond said.
“Generally, when there is a nationwide health care threat, people work in lockstep. And it's very confusing to me where this threat is actually happening, and we have sporadic implementation of protection for patients. And if I was somebody's daughter, and my dad went into hospital with a hip fracture and came out in a casket or had some kind of long-term disability from getting COVID in hospital when we know how to prevent it, I would be very mad at the system.”
Vipond said in an ideal world, there would be an independent third-party audit of the health system that would determine what is going wrong. But there are also proven, proactive measures that can prevent in-hospital transmission, such as universal masking, admissions testing, and recurrent testing of patients to guard against the “substantial proportion” of transmission that happens when people are asymptomatic.
“But instead, what seems to have happened is that our politicians, and therefore society, has decided that COVID is no longer an issue for anyone, and that includes vulnerable patients in hospitals.”
Many of the precautions Vipond mentioned were official health policy in the recent past, but rules around infection prevention have been relaxed or replaced altogether by the province’s health authorities.
AHS ended continuous masking requirements in its facilities and continuing care centres on June 19, 2023. Four months later, an enhanced masking directive was introduced, which can be activated by site leadership.
AHS did not respond to questions about how often the masking directive has been used since being adopted. Since Nov. 15, 2024, only three sites, Glenrose Rehabilitation Hospital, Misericordia Community Hospital, and Sturgeon Community Hospital, have had enhanced masking in effect, according to the AHS website.
During the early stages of the pandemic, Alberta moved fast to develop personal protective equipment standards and procedures for front-line health care workers, said Heather Smith, president of the United Nurses of Alberta (UNA). Though these agreements are still in place, AHS has updated several internal policies regarding COVID-19 measures.
Contact and droplet precautions no longer advise that staff within two metres of a patient with suspected or confirmed COVID-19 should utilize an N-95. And an updated return to work policy collapses COVID and other respiratory virus symptoms into a single directive, eliminated testing requirements and allowing employees to return to work within 24 hours of symptoms subsiding.
“The combination of these changes and attitudes towards COVID-19 have likely increased the risks health care workers face (due) to COVID-19 in their workplaces,” a spokesperson for UNA said in an email.
“There seems to be significant apathy among employers, and even among our membership in many cases, around COVID. And taking precautions is no longer seen as a priority, and maybe even not even seen as a necessity, which does create, in itself, its own risk,” Smith said.
Aside from the immediate disease outcomes, COVID infection has been linked to excess heart attacks, strokes, and more than 50 long-term effects that can linger for weeks or months after the initial infection. With health care workers facing elevated risk of catching COVID, the lasting impacts on workers and the industry are still emerging.
“We don't have long term experience in terms of the implications of multiple COVID exposures,” Smith said. “We don't know the liability that we are creating in terms of long-term or multiple exposure deficits and damages.”
An analysis of COVID claims from Alberta’s Workers Compensation Board shows that since the beginning of the pandemic, workers from municipal government, education, and health, which are reported together as one sector, have had more claims approved than any other sector.
The same trend can be seen in B.C.’s WorkSafe data, which shows 60 per cent of approved COVID claims come from health care and social services.
Vipond said there is an occupational health and safety obligation to protect staff from infections.
“It's not imaginary. It's in the legislation that we must protect all staff and all industries from preventable injury and illness. But for COVID, it really seems like that is no longer applicable. And because a substantial number of infections, even in young, healthy people, go on to cause long term illness . . . I really don't know why it's been allowed to continue to infect people at work.”
AHS said in a statement that it takes a variety of measures to safeguard the health and safety of patients and staff.
“When a unit is placed on outbreak, immediate actions are implemented, such as isolating symptomatic or patients with confirmed cases of respiratory viruses in designated rooms, placing visitation restrictions, and following rigorous infection prevention and control protocols,” the statement says.
“Outbreaks have occurred in acute care facilities both during periods of continuous masking and after the introduction of the enhanced masking directive. This enhanced masking directive is one of several tools used to prevent transmission, with decisions on its implementation made by zone and site leadership based on factors such as outbreak size, hospital occupancy, and test positivity rates. AHS continues to monitor and respond to outbreaks using evidence-based measures to minimize transmission and protect patients and staff.”